|
Personality disorders are mental conditions characterized by persistent patterns of thought, emotion, and behavior that deviate from cultural norms, causing difficulties in functioning and interpersonal relationships. These patterns are stable and inflexible, typically emerging in adolescence or early adulthood. Personality disorders are classified into three groups (clusters) according to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders).
Group A: Eccentric or Odd Disorders
Paranoid Personality Disorder: This disorder is characterized by intense suspicion and distrust of others, accompanied by the belief that others have malicious intentions. The individual is often wary, aggressive, and sensitive to criticism.
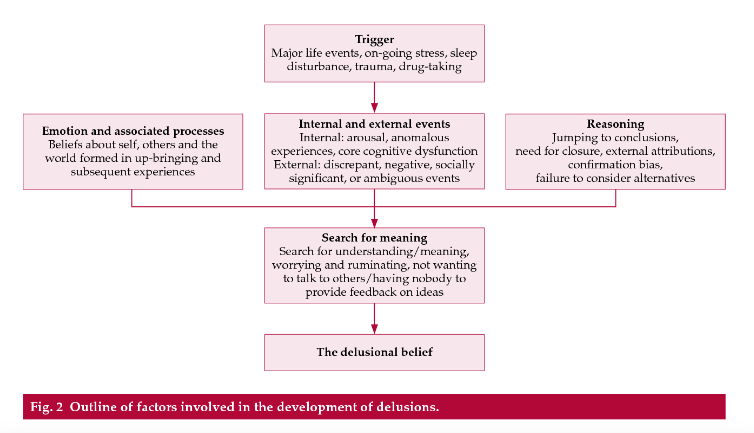
Outline Factors involved in the development of delusions by Freeman & Garety (2006).
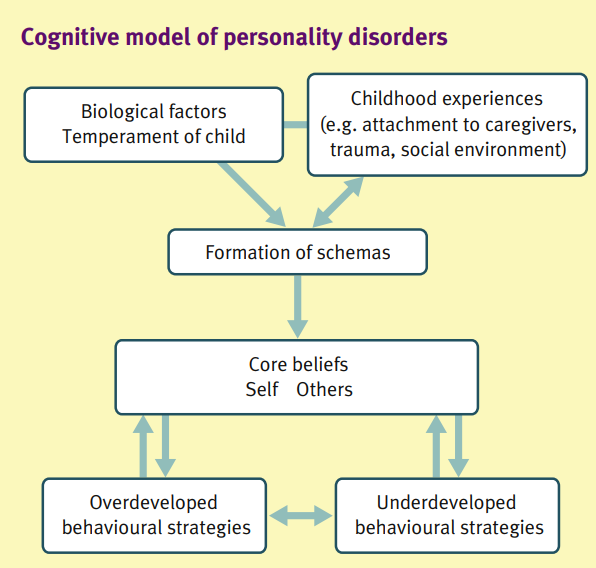
The Freeman & Garety (2006) model for Paranoid Personality Disorder (PPD) is a cognitive-behavioral framework that attempts to explain the development and maintenance of paranoid thoughts and beliefs. This model focuses on the connection between core beliefs, emotional states, and environmental perception, as well as the process through which paranoid beliefs become persistent and stable.
Key Elements of the Freeman & Garety Model (2006)
- Core Beliefs and Cognitive Schemas:
According to the model, individuals with paranoid personality disorder possess deeply rooted core beliefs and cognitive schemas that lead them to view the world as hostile and dangerous. These beliefs include ideas such as "Other people are malicious" or "You can't trust anyone."
These core beliefs influence how the individual interprets their experiences, leading to a consistent tendency toward paranoid thinking.
- Emotional Distress and Anxiety:
Emotional distress, such as anxiety, worry, and intense suspicion, plays a significant role in shaping paranoid beliefs. The model posits that individuals with high levels of anxiety and emotional distress are more likely to develop paranoid thoughts as a coping mechanism.
Anxiety enhances the tendency to interpret ambiguous situations as threatening, thus reinforcing paranoid beliefs.
- Interpretation of Ambiguous Situations:
A key element of the model is the interpretation of ambiguous or neutral situations as threatening. Individuals with paranoid tendencies tend to attribute malicious intentions to others even in situations where motives are unclear or there is no obvious threat.
This leads to a vicious cycle where paranoid thoughts are continually confirmed and reinforced.
- Suspicion and Lack of Trust:
The model emphasizes that paranoid personality disorder is characterized by a general lack of trust in others and heightened suspicion. These traits lead the individual to be constantly on guard for signs of threat or deception.
This tendency reinforces paranoid thoughts, as any minor deviation from what is expected or normal can be interpreted as an indication of threat.
- Confirmation of Paranoid Beliefs:
Once paranoid beliefs develop, the individual tends to seek confirmations for them, either by avoiding situations that could disprove them or by interpreting facts in ways that reinforce them. This can lead to a self-reinforcing cycle, where paranoid beliefs become increasingly stable and resistant to change.
- Social Isolation:
The model also highlights that paranoid thinking often leads to social isolation, as the individual avoids social interactions due to the belief that others are dangerous or malevolent. This isolation can further reinforce paranoid thoughts, as the individual lacks the opportunity to experience social interactions that could disconfirm their negative beliefs.
Interventions Based on the Freeman & Garety Model
Cognitive Behavioral Therapy (CBT) for Paranoid Personality Disorder, based on the Freeman & Garety model, includes the following strategies:
- Recognition and Modification of Paranoid Thoughts:
The therapy focuses on identifying paranoid thoughts and the core beliefs that underpin them. Patients are then trained to challenge these thoughts and consider alternative, more realistic explanations for their experiences.
- Anxiety Management:
Since anxiety plays a central role in the development and maintenance of paranoid thoughts, managing anxiety is a crucial part of the therapy. Techniques such as relaxation, mindfulness, and breathing training can help reduce anxiety and emotional distress.
- Social Skills Training:
Social isolation can reinforce paranoid beliefs. CBT may include social skills training to help individuals improve their social interactions and reduce isolation.
- Exposure to Ambiguous Situations:
Therapists may help patients gradually expose themselves to situations they consider ambiguous or threatening, with the goal of recognizing that these situations are not necessarily dangerous. This can help reduce paranoid perceptions.
- Restructuring Suspicion:
Therapists encourage patients to recognize and restructure excessive suspicion, guiding them toward a more balanced and realistic view of other people and their intentions.
Conclusion
The Freeman & Garety model (2006) offers a detailed understanding of the cognitive and emotional mechanisms contributing to the development and maintenance of Paranoid Personality Disorder. It emphasizes the interaction between deeply rooted core beliefs, anxiety, and the interpretation of ambiguous situations, as well as how paranoid thoughts become resistant to change. Cognitive Behavioral Therapy based on this model can help individuals with PPD modify their paranoid thoughts, reduce suspicion, and improve their social interactions.
2. Schizoid Personality Disorder:
This disorder involves a strong aversion to social relationships and a limited range of emotional expressions. Individuals with this disorder tend to be solitary, indifferent to social acceptance or rejection, and avoid intimacy.
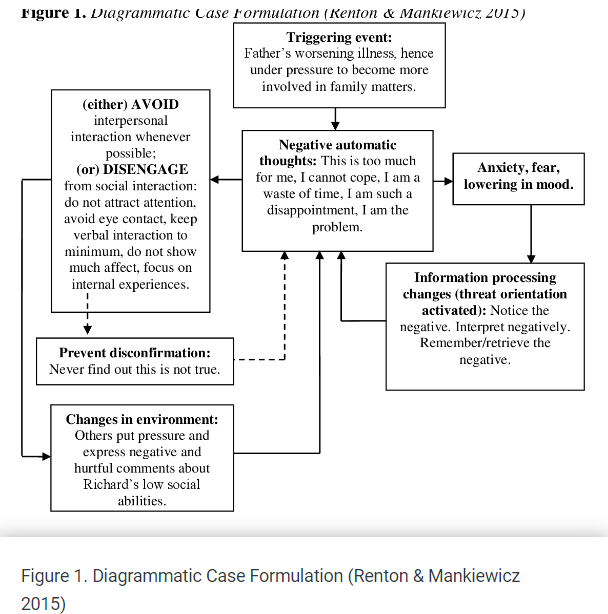
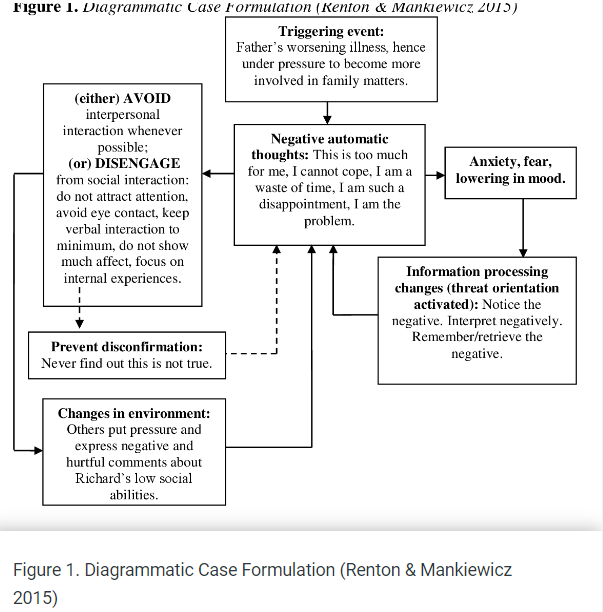
Schizoid Personality Disorder is a condition characterized by a disconnection from social relationships and a limited range of emotional expression in interpersonal interactions. Individuals with schizoid personality disorder tend to be isolated, avoid social relationships, and show indifference to criticism or affirmation from others.
Key Elements of the Cognitive Diagram for Schizoid Personality Disorder
- Core Beliefs and Cognitive Schemas:
Individuals with schizoid personality disorder develop core beliefs that lead them to withdraw from social relationships. Such beliefs may include thoughts like "Social relationships are meaningless" or "I am better off alone." These beliefs are deeply rooted and are associated with a general sense of indifference towards social interactions and living in social environments.
- Avoidance of Interpersonal Relationships:
A primary characteristic of schizoid personality disorder is the avoidance of interpersonal relationships. This is not necessarily due to a fear of social criticism or rejection, as seen in other disorders, but more to an internal belief that social relationships are unwanted or unnecessary. The individual may perceive interpersonal relationships as emotionally charged, chaotic, or difficult to manage, and therefore chooses to avoid them.
- Emotional Disconnection:
Individuals with schizoid personality disorder often exhibit emotional disconnection, meaning they struggle to express or experience intense emotions. This disconnection may include an inability to express love, anger, joy, or sadness, even in situations that would provoke emotional reactions in others. Emotional disconnection may arise from the belief that emotions are dangerous or pointless, reinforcing the tendency to avoid emotional bonds.
- Indifference to Social Validation:
Unlike other personality disorders, individuals with schizoid personality disorder do not seem to seek validation from others. They may show a noticeable indifference to criticism or acceptance from others because they do not consider social contacts important for their well-being. This indifference can lead to isolation and limited social interaction.
- Autonomy and Independence:
Individuals with schizoid personality disorder often develop a strong sense of autonomy and independence, based on the belief that they are self-sufficient and do not need others to fulfill their needs. This independence can lead to limited social relationships and isolation, but the individual does not perceive this as a problem, as they believe that this lifestyle aligns with their desires and needs.
Cognitive Model-Based Interventions for Schizoid Personality Disorder
Treatment for schizoid personality disorder may include the following strategies:
- Recognition and Modification of Core Beliefs:
Therapists assist individuals in recognizing their negative beliefs about social relationships and challenging them. This may involve exploring why social relationships are viewed as unnecessary or unwanted and developing new, more balanced beliefs.
- Enhancing Social Skills:
Social skills training can help individuals with schizoid personality disorder develop the ability to engage in social interactions in a way that is comfortable for them. This may include learning how to communicate effectively, express emotions, and develop and maintain relationships.
- Developing Emotional Awareness:
Therapy may focus on developing emotional awareness, meaning recognizing and expressing emotions. This can involve training in recognizing the physical and psychological signs of emotions and learning how to express them in a healthy manner.
- Self-Monitoring and Self-Awareness:
Patients are encouraged to observe their thoughts and reactions in social situations and examine how these thoughts influence their behavior. Self-monitoring can help identify thought patterns that lead to isolation and enhance the process of changing them.
- Gradual Exposure to Social Situations:
Gradual exposure to social situations can help individuals with schizoid personality disorder feel more comfortable with social interactions. Therapists can work with them to design steps for exposure to social situations in a manageable and less threatening way.
Conclusion
The cognitive model of schizoid personality disorder explains how deeply rooted negative beliefs about social relationships and emotional expression lead to isolation, emotional disconnection, and indifference to social validation. Therapeutic interventions based on this model aim to recognize and modify these beliefs, enhance social skills, and develop emotional awareness, helping individuals with schizoid personality disorder improve their functionality and quality of life.
3. Schizotypal Personality Disorder:
Characterized by odd thoughts, beliefs, or behaviors, as well as difficulties in forming close relationships. The individual may exhibit eccentric behavior, unorthodox perceptions (e.g., magical thinking), and challenges in social interaction.
Schizotypal Personality Disorder (SPD) is a psychiatric disorder characterized by significant social and interpersonal difficulties, odd thinking and behavior, as well as cognitive or perceptual distortions. Individuals with this disorder may exhibit strange beliefs or magical thinking, unusual sensory experiences, and social isolation. The cognitive model for schizotypal personality disorder provides an understanding of how cognitive distortions, perceptions, and beliefs contribute to the development and maintenance of the disorder.
Key Elements of the Cognitive Model for Schizotypal Personality Disorder
- Odd Beliefs and Magical Thinking: Individuals with schizotypal personality disorder often adopt strange or unusual beliefs and magical thinking. These beliefs may include ideas about telepathy, premonitions, or other forms of pseudoscientific beliefs. For example, a person might believe that their thoughts can influence events in a magical way or that they have special powers. These beliefs often arise from cognitive distortions, such as overgeneralization and erroneous attribution of causality, where the individual sees connections between events that are not actually linked.
- Cognitive and Perceptual Distortions: Schizotypal personality disorder is also characterized by cognitive and perceptual distortions. These may include distorted perceptions of the world or relationships, as well as strange sensory experiences. For instance, an individual might feel that there is a "presence" around them, even when nothing is there. Perceptual distortions and hallucinations, although not as pronounced as in schizophrenia, can affect how the individual perceives and interacts with their environment.
- Odd Behavior and Appearance: Individuals with schizotypal personality disorder may display odd or eccentric behavior and appearance. This behavior can include inappropriate or limited emotional expression, as well as unique habits or ways of communicating. The odd behavior may stem from the individual's attempt to manage their strange thoughts and perceptions or to express their unusual beliefs in a way they consider normal or necessary.
- Social Anxiety and Isolation: Social isolation and intense social anxiety are characteristic of schizotypal personality disorder. Individuals with this disorder often feel uncomfortable or inadequate in social situations, leading to avoidance of social contact. Their social anxiety may not diminish with familiarity with others, unlike what occurs in other disorders such as social phobia. The feeling of being different or misunderstood by others can reinforce this isolation and exacerbate social anxiety.
- Lack of Close Relationships: Individuals with schizotypal personality disorder often lack close relationships outside their family. This absence of relationships may be attributed to the feeling that others do not understand them or that they are too different from other people. This isolation may be reinforced by the avoidance of social contacts and a lack of trust in others, leading to a vicious cycle of isolation and the reinforcement of odd beliefs.
Cognitive Model-Based Interventions for Schizotypal Personality Disorder
- Therapeutic Focus: Treatment for schizotypal personality disorder based on the cognitive model may include the following strategies:
- Recognition and Modification of Odd Beliefs: The therapy focuses on recognizing strange or magical beliefs and questioning their accuracy and logic. Therapists assist individuals in developing more realistic and functional beliefs through cognitive techniques.
- Social Skills Training: Given the intense social anxiety and isolation observed in schizotypal personality disorder, social skills training is crucial. This may involve developing communication skills, understanding social cues, and managing social anxiety.
- Addressing Cognitive and Perceptual Distortions: Therapy may focus on reducing cognitive and perceptual distortions. This can be achieved through cognitive restructuring, where therapists help individuals recognize and modify their distorted thoughts and perceptions.
- Development of Anxiety Management Strategies: Since anxiety and social anxiety are pronounced in schizotypal personality disorder, training in anxiety management techniques, such as relaxation, mindfulness, and deep breathing, can be particularly beneficial.
- Gradual Exposure to Social Situations: Gradual exposure to social situations may help individuals confront social anxiety and improve their ability to interact with others. Therapists can work with individuals to design and implement strategies that allow them to engage in social activities with less anxiety.
Conclusion: The cognitive model of schizotypal personality disorder explains how odd beliefs, cognitive and perceptual distortions, social anxiety, and isolation combine to shape the core characteristics of this disorder. Therapeutic interventions focus on modifying these beliefs and developing social skills, helping individuals with schizotypal personality disorder improve their social interactions.
Group B: Dramatic, Emotional, or Unstable Disorders
- Borderline Personality Disorder (BPD):
This disorder is characterized by intense instability in interpersonal relationships, mood, and self-image. Individuals may experience profound fears of abandonment, impulsivity, self-destructive behaviors, and emotional instability.
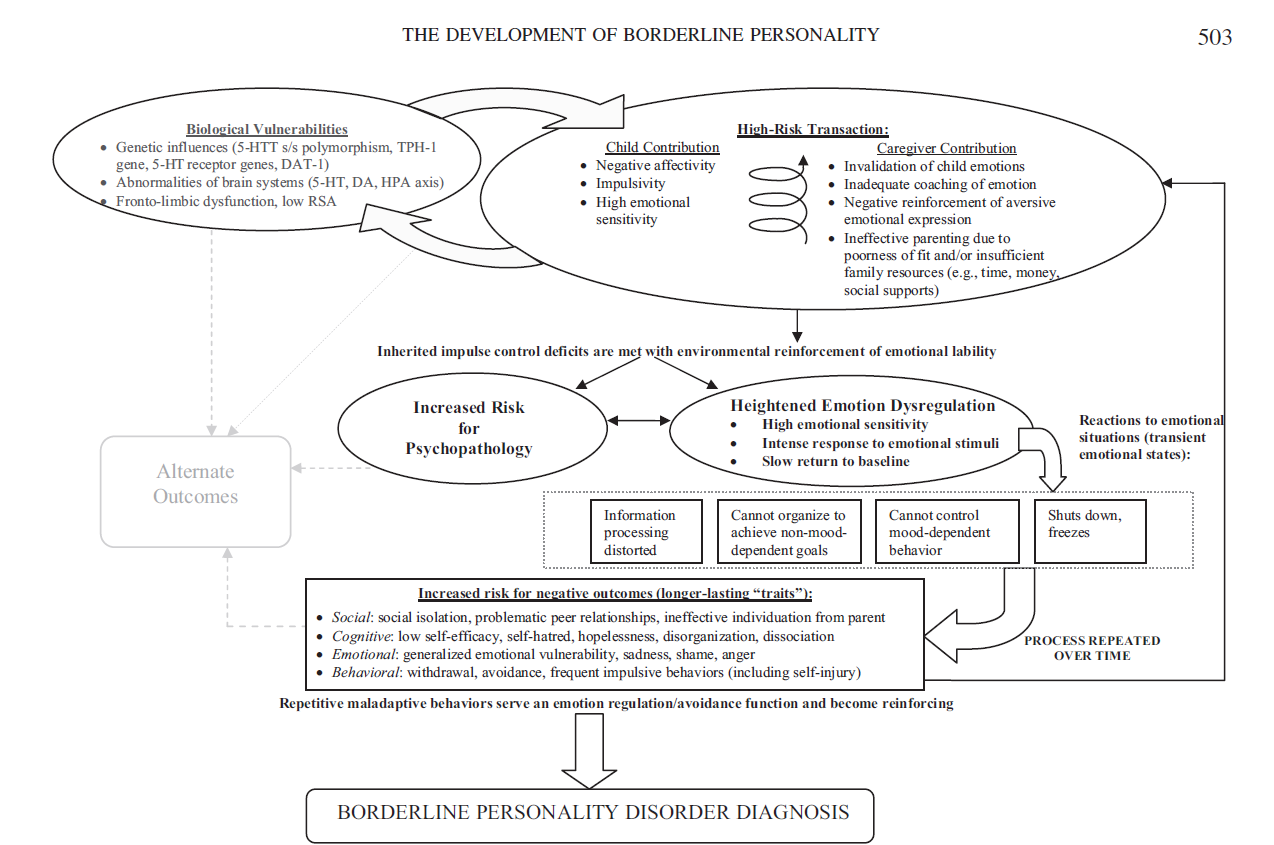
The cognitive model of Borderline Personality Disorder (BPD) by Crowell et al. (2009) is an important framework that seeks to explain the development and maintenance of this disorder through the interaction of genetic, psychological, and environmental factors. The model focuses on emotional dysregulation as the central mechanism that leads to the characteristic symptoms of BPD.
Key Elements of the Cognitive Model by Crowell et al. (2009) for Borderline Personality Disorder
- Emotional Dysregulation: Emotional dysregulation is the central pillar of Crowell et al.'s model for BPD. This dysregulation refers to the individual's inability to effectively regulate their emotions, leading to intense and unstable emotional reactions. Individuals with BPD often experience emotional states that are excessively intense, extreme, and difficult to manage. Emotional dysregulation can manifest as rapid mood swings, intense emotions such as anger, sadness, or anxiety, and difficulty returning to emotional equilibrium after a disturbance.
- Biological Vulnerability: According to the model, individuals with BPD may have biological vulnerabilities that make them more susceptible to emotional dysregulation. This vulnerability may include genetic factors, such as heredity or neurobiological anomalies, that affect how the individual processes and responds to emotions. Biological vulnerability may also involve dysfunctions in neurotransmitter systems involved in mood regulation, such as serotonin, or problems in brain development that impact executive functions and emotional self-regulation.
- Dysfunctional Environment: The model emphasizes the importance of a dysfunctional environment in the development of BPD. A dysfunctional environment, such as a family characterized by abuse, neglect, or instability, can reinforce the individual's emotional dysregulation. Parents or caregivers who are unable to provide stability, support, or validate the child's feelings may exacerbate the child's sense that their emotions are uncontrollable or lack value. The dysfunctional environment can also promote the development of insecure emotional bonds and encourage maladaptive behaviors as coping mechanisms for emotional distress.
- Interaction of Biological and Environmental Factors: Crowell et al. argue that the development of BPD results from the interaction between biological vulnerability and a dysfunctional environment. Individuals predisposed to emotional dysregulation may be more vulnerable to the negative effects of a dysfunctional environment, leading to the development of the characteristic symptoms of BPD. This interaction can create a vicious cycle where intense emotional dysregulation and unstable environmental responses reinforce each other, leading to a worsening of the disorder.
- Maladaptive Coping Mechanisms: Individuals with BPD often develop maladaptive coping mechanisms to manage their emotional dysregulation. These mechanisms may include self-harm, suicidal behaviors, explosive anger, or impulsive actions such as substance abuse. While these behaviors may provide short-term relief from the intensity of emotions, they ultimately exacerbate emotional instability and interpersonal conflicts, reinforcing the problems associated with BPD.
Interventions Based on the Cognitive Model by Crowell et al. (2009)
The treatment of BPD based on the Crowell et al. model includes various strategies, such as:
- Emotional Regulation Training: Since emotional dysregulation is central to BPD, training in emotional regulation is a key goal of therapy. This may involve learning techniques for recognizing and managing intense emotions, such as mindfulness, breathing techniques, and cognitive restructuring.
- Dialectical Behavior Therapy (DBT): DBT, a form of CBT specifically developed for BPD, focuses on teaching patients skills for emotional regulation, managing interpersonal relationships, and tolerating distress. DBT is particularly effective in addressing self-destructive behaviors and impulsive actions.
- Interpersonal Communication Skills Training: The therapy may include training in interpersonal communication skills, helping individuals with BPD improve their social relationships and reduce conflicts. This may involve learning ways to express their needs in healthy ways and managing interpersonal tensions.
- Trauma Processing: Since many individuals with BPD have a history of traumatic experiences, treatment may involve processing these experiences through techniques such as cognitive processing therapy or exposure therapy.
- Systemic Intervention: The therapy may also involve engaging the family environment or significant others in the therapeutic process to reduce environmental factors that exacerbate emotional dysregulation and enhance support for the individual.
- Narcissistic Personality Disorder: The individual has an excessive sense of self-importance, a need for admiration, and a lack of empathy for others. They often view themselves as superior to others and demand special treatment.
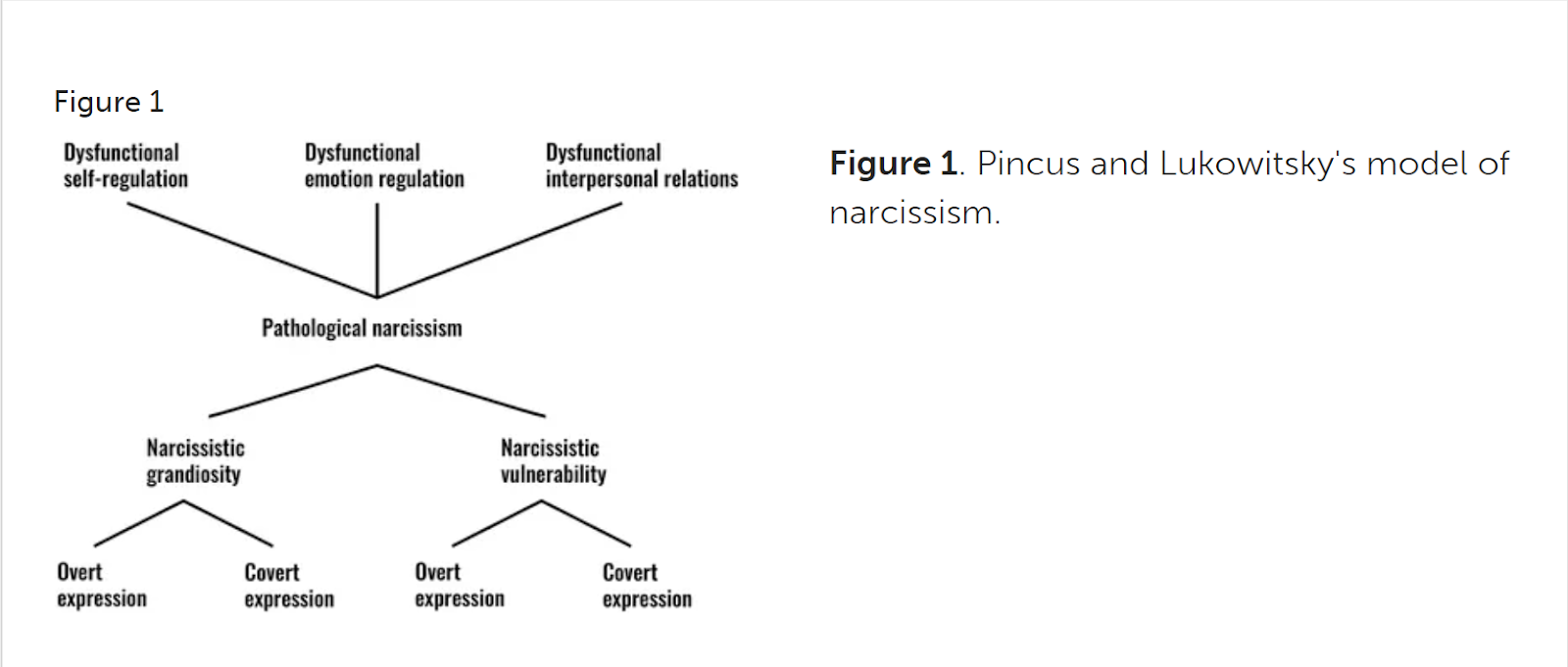
The Model of Pincus and Lukowitsky (2010) on Narcissism
The model by Pincus and Lukowitsky (2010) for narcissism is a multidimensional framework that seeks to explain the different manifestations of narcissism, including the fluctuations between seemingly contradictory traits, such as grandiose and vulnerable narcissism. This model recognizes that narcissism is not unidimensional but encompasses a range of behaviors, cognitive processes, and emotional experiences that may be expressed in various ways in different situations.
Key Elements of the Model by Pincus and Lukowitsky (2010)
Different Dimensions of Narcissism:
The model by Pincus and Lukowitsky proposes that narcissism can manifest through two primary dimensions: grandiose narcissism and vulnerable narcissism. Although these two dimensions are distinct, they can coexist within the same individual and alternate depending on the context and internal or external pressures.
- Grandiose Narcissism:
This is characterized by a strong sense of superiority, a need for admiration, and extroverted, flamboyant behavior. Individuals with this form of narcissism may be charming, ambitious, and continuously seek validation of their worth through external achievements and recognition.
- Vulnerable Narcissism:
This is marked by sensitivity to criticism, insecurity, and a hidden sense of inferiority. Individuals with vulnerable narcissism may experience intense anxiety and withdraw when they feel their self-image is threatened, even while maintaining a desire for admiration and recognition.
- Dynamic Alternation Between Grandiosity and Vulnerability:
One of the main points of the model is that the two dimensions of narcissism can alternate within the same individual. For example, a person may exhibit grandiose tendencies during periods of success or when feeling secure but may shift into a vulnerable state when facing failure or criticism. This alternation can be explained by the internal conflicts experienced by individuals with narcissistic tendencies, such as the need for admiration and a deeply rooted sense of insecurity.
- Psychological Defense and Self-Regulation:
The model emphasizes the use of psychological defenses and self-regulation strategies to maintain self-image. Individuals with grandiose narcissism may employ defenses such as projection, devaluation of others, or fantasies of success to protect their fragile self-esteem. In vulnerable narcissism, defenses may include avoidance, withdrawal, or excessive sensitivity to criticism. The constant need for external validation makes individuals susceptible to emotional fluctuations, especially when they do not receive the recognition they desire.
- Interaction with the Environment:
The model highlights that the expressions of narcissism are influenced by the individual's interactions with their environment. Feedback from the environment (e.g., criticism, praise, failure, or success) can enhance or diminish narcissistic tendencies. Social acceptance and success may amplify grandiose tendencies, while criticism and rejection may trigger vulnerability and anxiety.
- Relationships and Social Interactions:
Individuals with narcissistic tendencies often face challenges in interpersonal relationships. Grandiose narcissists may exploit or manipulate others to satisfy their need for admiration, while vulnerable narcissists may withdraw or be overly sensitive to interpersonal tensions. Social interactions often become difficult, as individuals with narcissism may demand excessive attention and validation or react intensely to perceived projections.
Interventions Based on the Pincus and Lukowitsky Model
Therapy for narcissism based on the Pincus and Lukowitsky model may include:
- Cognitive Behavioral Therapy (CBT):
CBT can assist individuals in recognizing and modifying cognitive distortions and beliefs that underpin narcissism, such as the need for constant admiration and the sense of superiority.
- Self-Regulation Training:
Therapists can train individuals in techniques for regulating their emotions and impulses, helping them cope with criticism and failure without resorting to dysfunctional behaviors.
- Development of Empathy and Social Skills:
Since narcissism is often associated with a lack of empathy, therapy may focus on cultivating empathy and interpersonal communication skills, improving relationships and reducing conflicts.
- Exploration of Insecurity and Self-Esteem:
In cases of vulnerable narcissism, therapy may involve exploring the deep-seated insecurity and low self-esteem underlying the need for admiration, assisting individuals in developing a more stable and healthy self-image.
- Addressing the Interaction Between Dimensions:
Therapy may also focus on understanding and addressing the oscillation between grandiosity and vulnerability, helping individuals cultivate a more consistent and stable identity.
2. Histrionic Personality Disorder
This disorder is characterized by an intense need for attention and validation, along with dramatic or provocative behavior. Individuals with this disorder are often overly emotional and seek attention through theatrical behaviors or charm.
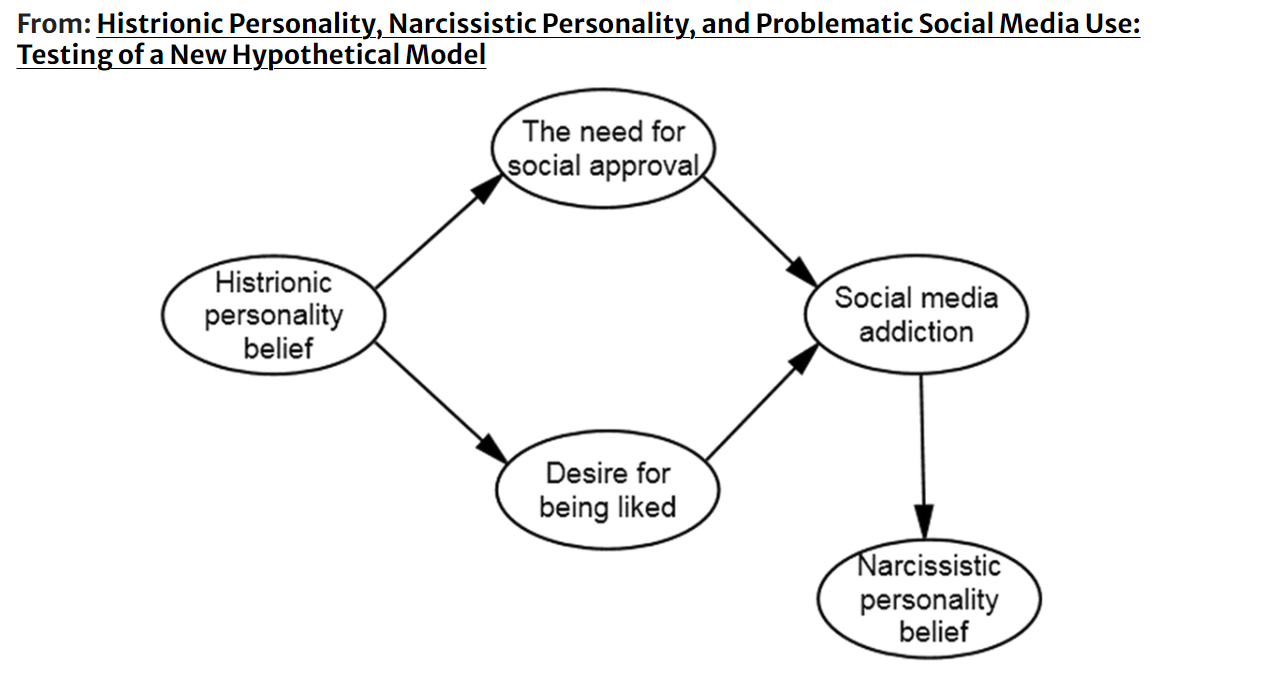
Cognitive Model of Histrionic Personality Disorder (HPD)
The cognitive model for Histrionic Personality Disorder (HPD) offers an understanding of the disorder by analyzing the core beliefs, cognitive schemas, and behavioral patterns that characterize individuals with this condition. HPD is marked by excessive emotionality, a need for attention, and dramatic behavior. The cognitive model focuses on how these cognitive processes and behaviors develop and are sustained over time.
Key Elements of the Cognitive Model for Histrionic Personality Disorder
-
Core Beliefs and Cognitive Schemas:
Individuals with Histrionic Personality Disorder (HPD) possess core beliefs centered around the need to be the focus of attention. They may hold deeply rooted thoughts such as, "I must attract attention to be worthy" or "If others don’t pay attention to me, I am insignificant." These beliefs lead to the development of cognitive schemas that reinforce dramatic and emotionally exaggerated behaviors, as well as a dependence on external validation for their self-esteem.
-
Attention and Validation Seeking:
The need for attention and validation is central to the cognitive model of HPD. Individuals with this disorder often seek constant affirmation from others, employing excessive emotional expressions, charm, and dramatic reactions to capture attention. This ongoing need for validation can result in superficial relationships, where genuine emotional connection is hard to achieve, as the individual focuses more on being the center of attention rather than cultivating deep and stable relationships.
-
Superficial Emotional Expression:
People with HPD tend to exhibit exaggerated but superficial emotions. They may express intense feelings, such as excitement, sadness, or anger, without necessarily experiencing the same intensity internally. This superficial emotional expression is linked to the belief that dramatically presenting their emotions will help them gain the attention and validation they crave.
-
Interpersonal Difficulties:
The cognitive model highlights the challenges faced by individuals with HPD in their interpersonal relationships. Due to their need to be the center of attention, they may overlook the needs of others or become excessively dependent on others for their validation. This behavior can lead to conflicts, as others may feel that their relationships with the individual with HPD are superficial or one-sided.
-
Pursuit of Drama and Adventure:
Individuals with HPD often seek out dramatic situations and adventures, as these provide them with opportunities to be in the spotlight. They may pursue new experiences or exaggerate their stories to appear more interesting to others. This quest for drama can result in impulsive decisions or behaviors that have negative consequences, yet individuals with HPD often prioritize the immediate attention they receive over long-term repercussions.
Interventions Based on the Cognitive Model for Histrionic Personality Disorder
The treatment of Histrionic Personality Disorder (HPD) based on the cognitive model may include various strategies:
-
Recognition and Modification of Core Beliefs:
Therapy focuses on identifying negative core beliefs that contribute to the excessive need for attention and validation. Therapists assist individuals in understanding how these beliefs influence their behavior and help them develop more realistic and healthier beliefs about themselves and their relationships.
-
Emotional Self-Regulation Training:
Given that individuals with HPD often express emotions in exaggerated and superficial ways, therapy may involve training in emotional self-regulation. This includes techniques for recognizing and authentically expressing emotions, as well as learning how to tolerate rejection or criticism without resorting to dramatic reactions.
-
Development of Interpersonal Skills:
Therapy may include training in interpersonal skills, aiding individuals with HPD in forming and maintaining more meaningful and balanced relationships. This can involve learning to listen and respond to the needs of others and recognizing when their behaviors may be excessive or lead to conflicts.
-
Reframing the Need for Attention:
Therapy can help individuals reframe their need for attention by showing them how to seek validation and express their individuality in more functional ways, without resorting to excessive or dramatic behavior.
-
Addressing Insecurity and Low Self-Esteem:
Often, the excessive need for attention and dramatic behavior stem from deeper insecurities and low self-esteem. Therapy can focus on enhancing self-esteem and developing a more stable and healthy self-image.
Conclusion
The cognitive model for Histrionic Personality Disorder offers insight into how core beliefs and cognitive schemas lead to an excessive need for attention, dramatic behavior, and superficial interpersonal relationships. Through therapy, individuals with HPD can recognize and modify these beliefs, develop healthier ways to express their emotions, and improve their interpersonal relationships, ultimately leading to a more fulfilling and balanced life.
Antisocial Personality Disorder:
Antisocial Personality Disorder is characterized by a persistent violation of the rights of others, a lack of remorse or guilt, irresponsibility, and indifference to the safety of others. Individuals with this disorder often engage in antisocial or criminal activities.
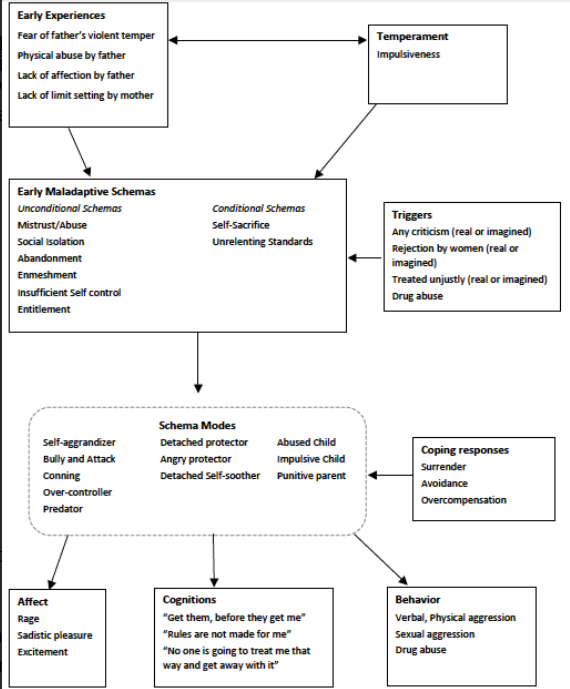
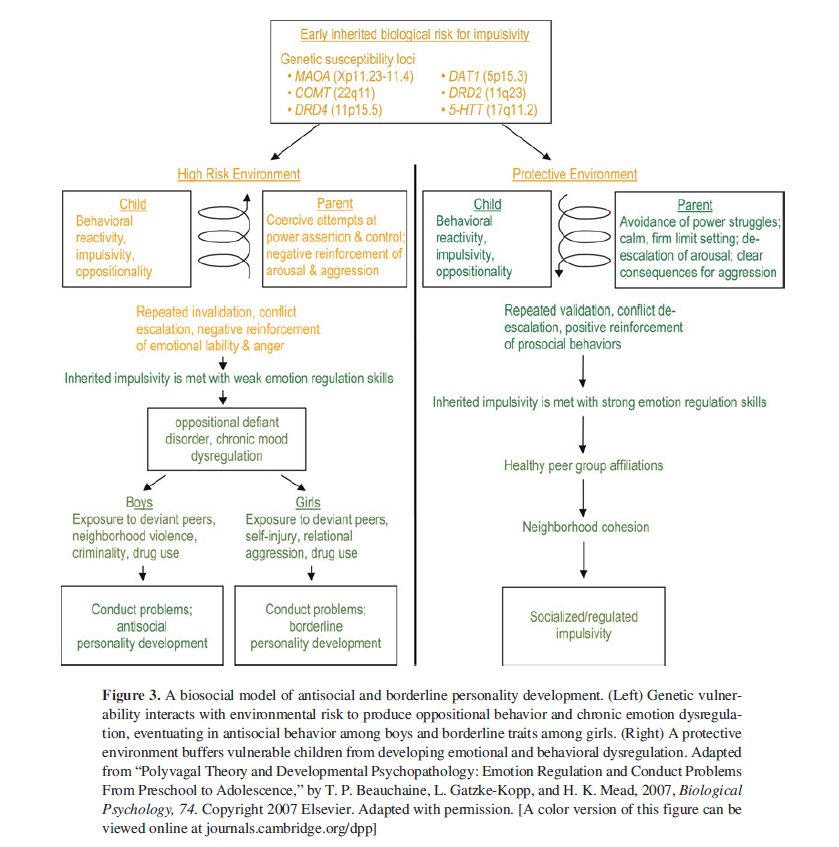
The cognitive model of Antisocial Personality Disorder (ASPD), developed by T. P. Beauchaine, L. Gatzke-Kopp, and H. K. Mead in 2007, seeks to explain the development and maintenance of antisocial behavior through the interaction of biological, psychological, and environmental factors. This model focuses on the key cognitive and emotional processes that characterize antisocial personality and the associated behaviors.
Key Elements of the Cognitive Model by Beauchaine, Gatzke-Kopp, and Mead (2007)
- Biological Vulnerability and Neurobiology:
The model begins by recognizing biological vulnerability as a key factor contributing to the development of Antisocial Personality Disorder (ASPD). According to Beauchaine and colleagues, biological abnormalities, such as dysfunction in brain systems involved in emotional regulation and impulsivity (e.g., the dopamine system), play a significant role. This biological vulnerability may include differences in the functioning of the prefrontal cortex, which is responsible for executive function and impulse control, as well as abnormalities in the amygdala, which is related to emotional processing and fear response.
- Cognitive Distortions and Perceptions:
The cognitive model emphasizes that individuals with ASPD often exhibit cognitive distortions that affect their perception and interpretation of social situations. These distortions may include a tendency to view others as weak or deserving of exploitation, underestimating the feelings of others, and lacking guilt or remorse for their antisocial actions. These cognitive processes lead to the development of a mindset that justifies aggressive or exploitative behavior, minimizing moral responsibility or the impact of their actions on others.
- Emotional Dysregulation and Impulsivity:
Individuals with ASPD frequently struggle with emotional regulation and display high levels of impulsivity. Emotional dysregulation may manifest as increased irritability, anger, or an inability to control impulsive behavior, often resulting in aggressive or violent acts. This emotional instability is closely linked to biological vulnerability and is reinforced by cognitive distortions that render antisocial behaviors acceptable or even necessary.
- Environmental Factors and Social Learning:
The model by Beauchaine and colleagues also acknowledges the importance of environmental factors in the development of ASPD. Individuals with this disorder often grow up in environments where aggression, violence, or criminality are normalized behaviors. Such environments may reinforce antisocial tendencies through social learning, where children learn to resolve conflicts or achieve their goals through aggressive or exploitative actions. Dysfunctional family relationships, lack of parental supervision, and frequent experiences of abuse or neglect are also critical factors contributing to the development of the disorder.
- Lack of Empathy and Moral Development:
A significant aspect of the model is the lack of empathy that characterizes individuals with ASPD. This lack of empathy, combined with insufficient moral development, allows these individuals to exploit or harm others without experiencing guilt or remorse. Moral development in individuals with ASPD is often inadequate, and their actions are driven by immediate needs and desires rather than the social or moral consequences of their behavior.
Interventions Based on the Cognitive Model by Beauchaine, Gatzke-Kopp, and Mead
The treatment of Antisocial Personality Disorder (ASPD) based on this model may involve various strategies:
- Cognitive Restructuring:
Therapy can focus on recognizing and modifying the cognitive distortions that lead to antisocial behavior. Therapists assist individuals with ASPD in understanding their misconceptions and developing more functional thought patterns that consider the consequences of their actions on others.
- Emotion Regulation Training:
Training in emotional self-regulation is crucial for individuals with ASPD, as it can help them manage their emotional dysregulation and impulsivity. Developing skills to recognize emotions, tolerate distress, and prevent impulsive behavior are key goals of therapy.
- Empathy Development and Moral Understanding:
Therapy may include empathy training, helping individuals with ASPD understand the emotions and experiences of others. This can contribute to the development of a better moral understanding and deter antisocial behaviors.
- Systemic Intervention and Family Therapy:
Given the role of environmental factors in the development of ASPD, family therapy and systemic interventions can help improve family relationships and reduce factors that reinforce antisocial behavior.
- Enhancing Social Skills and Compliance with Rules:
Training in social skills and enhancing compliance with social norms can help individuals with ASPD improve their relationships and better adapt to social demands.
Group C: Anxiety or Phobic Disorders
1. Avoidant Personality Disorder
This disorder is marked by a strong fear of criticism, disapproval, or rejection, leading to social avoidance and feelings of inadequacy. Individuals with this disorder desire social relationships but fear rejection or disapproval.
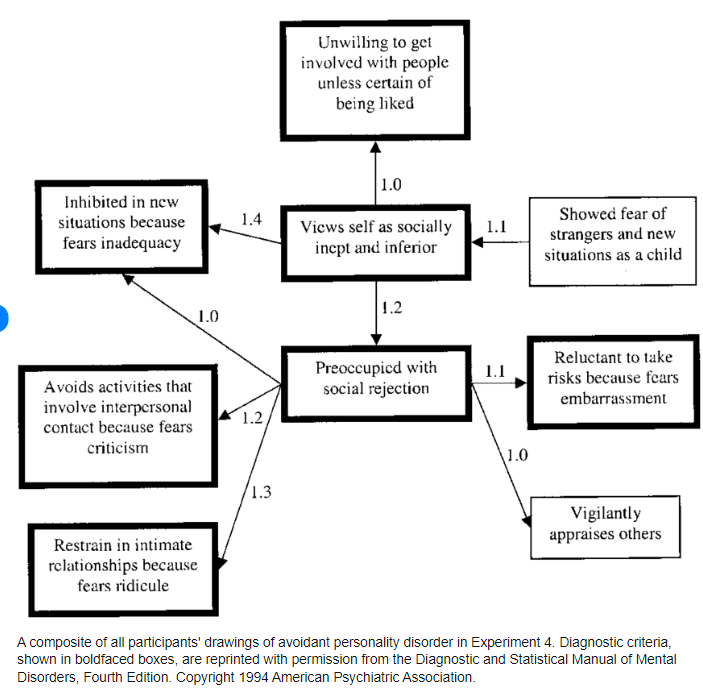
Nansy S. Kim, along with other psychologists and researchers, has made significant contributions to understanding Avoidant Personality Disorder (AvPD) through the development of a cognitive model that explains the disorder's development and maintenance. AvPD is characterized by an intense fear of social rejection, excessive self-consciousness, and avoidance of social situations due to fear of humiliation or criticism.
Key Elements of the Cognitive Model of Avoidant Personality Disorder
- Core Beliefs and Cognitive Schemas:
Individuals with Avoidant Personality Disorder (AvPD) have deeply rooted negative beliefs about themselves and their social abilities. These beliefs often include thoughts such as "I am inadequate" or "I don't deserve to be accepted." These negative beliefs lead to the formation of cognitive schemas that reinforce low self-esteem, creating a self-perpetuating system of negative thoughts and behaviors. These core beliefs influence how the individual interprets social situations, often perceiving interactions with others as threatening or demeaning.
- Fear of Rejection and Criticism:
One of the main characteristics of AvPD is the intense fear of rejection and criticism from others. Individuals with this disorder believe that they will be rejected or judged negatively in social situations, which leads them to avoid these situations to protect themselves from the perceived threat. This fear often stems from negative experiences in the past, where the individual may have faced rejection, ridicule, or humiliation. These negative experiences reinforce dysfunctional beliefs and fuel avoidance behavior.
- Avoidance as a Coping Mechanism:
Avoiding social situations is a central coping mechanism for individuals with AvPD. By steering clear of situations where they might feel insecure, be rejected, or criticized, individuals with AvPD reduce immediate discomfort, but this comfort-maintaining strategy ultimately reinforces dysfunctional beliefs and social isolation in the long run. Avoidance not only sustains the negative self-image but also prevents opportunities for positive social experiences that could challenge the individual’s dysfunctional beliefs.
- Self-Fulfilling Prophecies:
The model emphasizes the role of self-fulfilling prophecies in AvPD. Negative beliefs about oneself and social interactions lead the individual to expect rejection or criticism in every social encounter. These expectations result in behaviors such as withdrawal or an inability to engage actively in conversations, which can provoke negative reactions from others and reinforce the individual’s initial beliefs. Thus, the individual's expectations and behaviors lead to a self-reinforcing process where the negative self-image and fear of rejection are continuously validated.
- Low Self-Esteem and Social Isolation:
Low self-esteem is a central characteristic of AvPD. Individuals with this disorder often feel incapable and unworthy, leading to increased social isolation. Avoiding social contact further diminishes self-esteem, as individuals do not receive the necessary social support and positive feedback. Social isolation, in turn, reinforces the belief that the individual is unacceptable or does not deserve to belong to social groups.
Interventions Based on the Cognitive Model of AvPD
Treatment for Avoidant Personality Disorder (AvPD), based on Nancy S. Kim's cognitive model, may include the following strategies:
- Cognitive Restructuring:
Therapy can focus on recognizing and modifying the dysfunctional beliefs that underpin the fear of rejection and social avoidance. Through cognitive restructuring, the individual is encouraged to challenge their negative thoughts and develop more realistic and positive beliefs about themselves and others.
- Social Skills Training:
Social skills training is critical for individuals with AvPD. Learning how to engage in conversations, recognize and respond to social cues, and develop and maintain relationships can help reduce social anxiety and enhance self-confidence.
- Self-Esteem and Self-Acceptance:
Enhancing self-esteem is a central goal of therapy. The treatment can help the individual recognize their positive qualities, develop self-acceptance, and reduce excessive self-criticism.
- Gradual Exposure to Social Situations:
Gradual exposure to social situations can help the individual overcome the fear of rejection and build confidence in social interactions. This approach involves progressively participating in anxiety-provoking situations, starting with the least threatening and moving on to more challenging ones.
- Development of Anxiety Management Strategies:
Therapy may include anxiety management techniques, such as relaxation, breathing exercises, and mindfulness, to help the individual cope with anxiety related to social interactions.
Conclusion
Nancy S. Kim's cognitive model of Avoidant Personality Disorder (AvPD) provides a clear and comprehensive approach to understanding how dysfunctional beliefs, fear of rejection, social avoidance, and low self-esteem interact and contribute to the development and maintenance of the disorder. Through targeted therapeutic interventions, individuals with AvPD can recognize and modify these dysfunctional thoughts into new, more functional ones.
3. Dependent Personality Disorder
The individual has a strong need to receive care from others and experiences excessive fear of abandonment or rejection. It is characterized by submissive behavior and difficulty in making decisions without the reassurance of others.
Dependent Personality Disorder (DPD) is characterized by a strong and pervasive need for care from others, which leads to submissive and clingy behavior and fear of separation. The cognitive model for dependent personality disorder provides an understanding of the dysfunctional beliefs and cognitive schemas that lead to this behavior.
Key Elements of the Cognitive Model for Dependent Personality Disorder
- Core Beliefs and Cognitive Schemas:
Individuals with dependent personality disorder often have deeply rooted beliefs that they are incapable of taking care of themselves or making decisions without the help of others. These core beliefs may include thoughts such as "I am weak" or "I cannot survive without others." These beliefs create cognitive schemas that guide the individual's behavior, leading them to constantly seek support, affirmation, and guidance from others.
- Fear of Independence and Separation:
One of the main features of DPD is the intense fear of independence and separation. Individuals with this disorder often feel significant insecurity when faced with the possibility of being alone or having to make decisions without the help of others. This fear leads to clingy behavior, as individuals try to ensure that they will not be left alone and that they will always have someone to care for them or guide them.
- Submissive and Passive Behavior:
Submissive and passive behavior is characteristic of DPD. Individuals with this disorder often yield to the desires of others, even if it means neglecting their own needs or wishes. This behavior stems from the belief that maintaining relationships is more important than expressing their own opinions or desires. Individuals with DPD may fear that if they do not agree or submit, others will reject or abandon them.
- Seeking Affirmation and Support:
Individuals with dependent personality disorder constantly seek affirmation and support from others. This need arises from the insecurity they feel about their abilities and their inability to handle situations on their own. The ongoing search for affirmation can lead to a vicious cycle, where the individual becomes increasingly dependent on others and loses confidence in their ability to face challenges independently.
- Difficulty Making Decisions:
Individuals with DPD often struggle to make decisions without the advice or approval of others. Their inability to make decisions may stem from deeply ingrained beliefs that they are incapable or that they will make mistakes if they do not have someone else's help. This difficulty in decision-making reinforces their dependence on others and their constant search for guidance.
Interventions Based on the Cognitive Model for Dependent Personality Disorder
The treatment of dependent personality disorder, based on the cognitive model, may include various strategies:
- Cognitive Restructuring:
Therapy can focus on recognizing and modifying dysfunctional beliefs related to incapacity and dependence. Through cognitive restructuring, individuals are encouraged to develop a more positive and realistic perception of their abilities and self-sufficiency.
- Enhancing Self-Confidence:
Therapy may focus on building self-confidence, helping individuals recognize their own capabilities and take initiatives without constantly seeking affirmation from others.
- Decision-Making Training:
Decision-making training is critical for individuals with DPD. Therapy may involve learning techniques to develop autonomy in decision-making, starting with simple daily decisions and progressing to more complex ones.
- Developing Independence:
Therapy can help individuals develop independence skills, such as managing their daily needs and taking on responsibilities without continually relying on others for guidance and support.
- Managing the Fear of Rejection:
Therapy may focus on addressing the fear of rejection and abandonment. This can include developing strategies for managing emotions arising from the fear of losing relationships and enhancing the individual’s ability to maintain relationships without being overly dependent.
Conclusion
The cognitive model for Dependent Personality Disorder explains how dysfunctional beliefs about incapacity and the need for constant support lead to clingy behavior, submissiveness, and difficulty in decision-making. Through therapy, individuals with DPD can recognize and modify these beliefs, develop self-confidence and independence, and improve their ability to manage their lives with greater autonomy and self-sufficiency.
4. Obsessive-Compulsive Personality Disorder (OCPD):
Characterized by a strong need for order, perfectionism, and control, with an emphasis on details, rules, and organization. Individuals with OCPD are often rigid, perfectionistic, and have difficulty relaxing or relinquishing control.
Personality disorders typically require specialized treatment, such as psychotherapy (e.g., cognitive-behavioral therapy, dialectical behavior therapy) and, in some cases, medication to address symptoms of anxiety or depression.
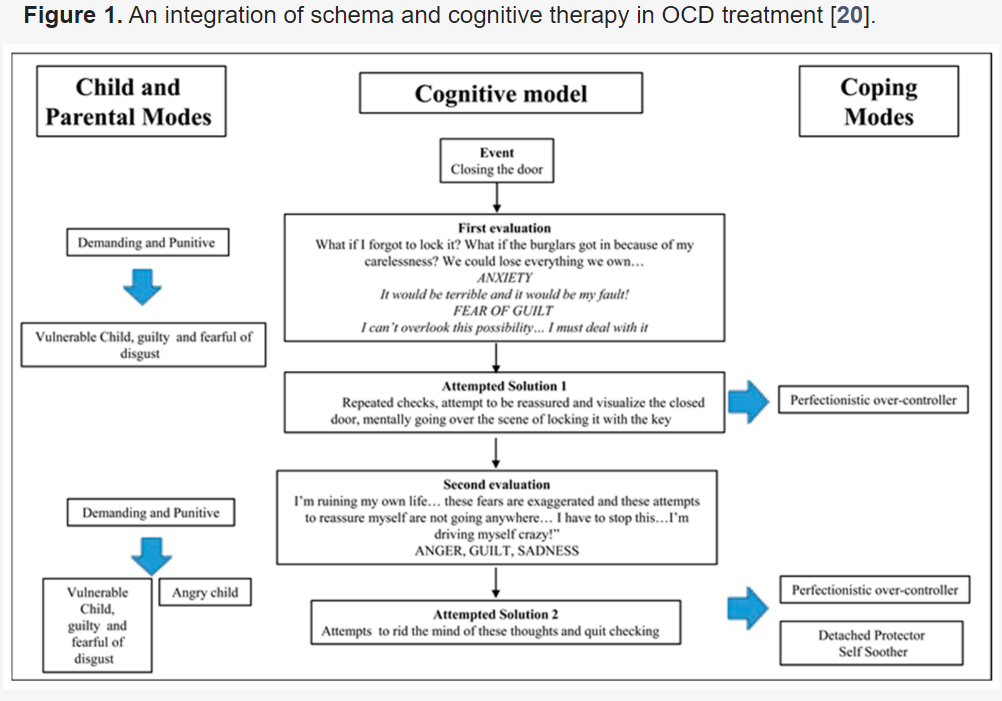
Cognitive Model for Obsessive-Compulsive Personality Disorder (OCPD)
Obsessive-Compulsive Personality Disorder is characterized by excessive preoccupation with order, perfectionism, and control, which affects the individual's flexibility and efficiency, as well as their interpersonal relationships. The cognitive model of OCPD focuses on how dysfunctional beliefs and cognitive schemas lead to compulsive and rigid behavior.
Key Elements of the Cognitive Model of OCPD
- Core Beliefs and Cognitive Schemas:
Individuals with OCPD have deeply ingrained beliefs that order, perfection, and control are necessary to avoid failure or criticism. These beliefs may include thoughts like "If everything isn't perfect, I'll fail" or "I must control everything to avoid chaos."
These beliefs lead to the creation of cognitive schemas that direct the individual's behavior toward the pursuit of perfection and strict adherence to rules and standards, even if this causes dysfunction or anxiety.
- Perfectionism and Rigidity:
One of the main characteristics of OCPD is excessive perfectionism. Individuals with this disorder set extremely high standards for themselves and others, often feeling intense anxiety when they cannot meet these standards.
This perfectionism can lead to rigidity and inflexible behaviors, as the individual attempts to maintain control and order in every area of their life. This may manifest in excessive attention to detail, inflexibility regarding rules and order, and difficulty adapting to changes or unpredictable situations.
- Excessive Control:
The need for control is central to OCPD. Individuals with this disorder often feel they must control every aspect of their lives to prevent failure, criticism, or chaos. This need for control may also extend to others, as individuals with OCPD attempt to impose their views and rules on those around them.
The excessive need for control can create problems in interpersonal relationships, as others may feel restricted or oppressed by the demands and expectations of the person with OCPD.
- Fear of Failure and Criticism:
One of the main motivators behind perfectionism and control in OCPD is the fear of failure and criticism. Individuals with this disorder often believe that if they do not achieve their high goals or maintain absolute control, they will fail and face negative criticism or rejection.
This fear leads to constant anxiety and excessive effort to avoid situations where failure or negative evaluation may occur.
- Dysfunctional Relationships:
Due to perfectionism, rigidity, and the need for control, individuals with OCPD often struggle to develop and maintain healthy interpersonal relationships. Others may perceive them as overly critical, inflexible, or impatient, which can lead to conflicts or distancing.
The difficulty in understanding and accepting the needs and feelings of others can exacerbate relationships, as individuals with OCPD focus more on rules and structure than on emotional needs and companionship.
Interventions Based on the Cognitive Model for OCPD
Treatment for OCPD based on the cognitive model may include the following strategies:
- Cognitive Restructuring:
Therapy may focus on identifying and modifying dysfunctional beliefs related to perfectionism, control, and failure. Therapists help individuals develop more realistic and flexible beliefs that reduce anxiety and the need for absolute control.
- Flexibility Training:
Therapy can assist individuals with OCPD in developing flexibility in their thinking and behavior. This may include training in accepting uncertainty, tolerating failure, and adapting to changes and unpredictable situations.
- Addressing Fear of Failure:
Therapy can help individuals confront their fear of failure and criticism, encouraging them to recognize that failure is part of the human experience and does not diminish their worth as individuals.
- Development of Interpersonal Skills:
Therapy may include training in interpersonal skills, helping individuals with OCPD improve their relationships with others. This can involve learning to recognize and respond to the emotional needs of others, as well as enhancing communication and empathy.
- Anxiety Management Training:
Since anxiety is often intense in OCPD, therapy may include anxiety management techniques such as relaxation, breathing exercises, and mindfulness to help the individual cope with the anxiety arising from the need for perfection and control.
|